Mandibular Advancement Splints
TYPES OF MANDIBULAR ADVANCEMENT SPLINTS AND DEVICES
There are many different types of appliances available on the market.
A mandibular advancement splint should be tailored to the patient’s individual problems by a dentist experienced in making these devices.
Appliances fall into three main groups.
1. DUOBLOCK FULLY ADUSTABLE APPLIANCES – UPPER AND LOWER SEPERATE MEMBERS
Various designs exist that allow adjustments in protrusive and lateral jaw movements. Adjustments allow the lower jaw to be moved more forward over time allowing you to get used to the appliance slowly.
A.) Ramps. The lower appliance has wings that slide against a ramp on the upper appliance to shunt the lower jaw forward. There is no mechanical connection between upper and lower members allowing the patient to open their mouth, talk and drink. These appliances seem to be favoured by patients. The Somnomed Mandibular Advancement Splint is shown below.
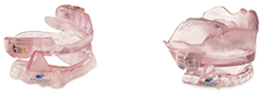

- Adjustment mechanism on upper Somnomed appliance

- Somnomed MAS allows patients to open their mouths.
Although many different designs are available, the most common appliances made in Australia are the Somnomed and the MDSA patterns.
B.) Mechanical locking mechanism.- These devices usually allow some lateral jaw movement but patients can not readily talk or drink wearing these devices as both top and bottom members are mechanically connected together.
MDSA type of mandibular advancement splint shown below.

2. Two Pieces Non Adjustable -Duoblock
These are custom made devices made by the dentist on the patient’s impressions where the top and bottom members are fused together. These devices fit well and are relatively inexpensive. These devices are not advisable as they can not be adjusted without returning to the laboratory.
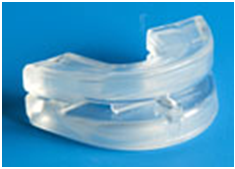
3. Boil and Bite – one piece non adjustable
Non adjustable monoblock (one piece) thermoplastic devices are available over the Internet. The patient has to make their own appliances by boiling the material in a pot at home and biting into the material in the correct position and moulding the material while it sets. This technically difficult to manage.
Although very inexpensive these devices are:-
- Not adjustable
- Are extremely difficult for a patient to make these appliances to fit their own mouth and to establish the correct bite position.
- Home made appliances fit poorly and tend to fall out when bitten on.
- The appliance loosens and is unstable over time as the material is relatively soft and distorts.
- Most patients give up wearing them because of instability. Studies show only about 17% of people tolerate these appliances.
WHAT TO EXPECT
Most patients are happy with their MAS within a week and prefer to sleep with the device rather than be without their splints.
Many patients report that they are now sleeping with their partners in the same room again, are getting a better night’s sleep, are less tired and feel confident about going away on holidays with other people.
Advantages:
Non surgical, safe, no pain, effective, unobtrusive, well researched with good patient acceptance. Appliances are small and easily transportable. Require no electricity or supplies. Relatively buy tramadol pain online inexpensive and lasts for years. Has greater patient acceptance than CPAP and quieter than CPAP.
Disadvantages:
Temporary discomfort, dry mouth, excess saliva, rarely pain to the jaw which is passes. A small percentage, about 7% of patients may have alterations to jaw and bite resulting in an open bite on their back teeth. If the appliance is left out the bite will return to normal. Nearly all these small group of patients elect to continue wearing the appliance as the open bite does not bother the patient and feel much better for wearing the appliance.
WHAT TO EXPECT DURING YOUR VISITS
First Visit: During this visit the patient is examined to ensure MAS therapy will be effective. Teeth with decay must be restored before making the MAS as the appliance rests on top of the teeth and altering the shape of the teeth after the device is made may make the MAS not fit properly.
- Gum problems have to be treated prior to any device being placed in the mouth as all oral appliances affect cleaning and salivary flow may make gum conditions worse.
- The mouth is checked for decay and poor fillings. All new fillings should be completed before impressions are taken for an MAS. The appliance may not fit if a number of large fillings or crowns are needed after the appliance is made.
- The occlusion, jaw joints, jaw movements are checked and recorded.
- Mimicked snore sounds are noted in different body positions and recorded.
- Epworth questionaire: assesses the liklihood of having obstructive sleep apneoa in addition to snoring
- Assessemnt of oropharangeal space is made.
If the patient is found suitable for treatment bite registration records and impressions are taken.
Second Visit: The MAS is fitted at a second visit two to three weeks later.
Third Visit:A follow up visit is made at one week where the appliance is checked and adjusted if required. Despite MAS’s initial bulk it usually takes only one week to become used to the appliance.
Most patients report a dramatic decrease in snore sounds and both sleeping partners and patients are happy with the results. Some patients admit that they are now sleeping in the same room again. Many patients report they are getting a better night’s sleep and feel more refreshed in the morning.
Fourth Visit: A one month follow up appointment is scheduled by which time patients are completely used to the MAS. At this time, it is my usual practice to arrange a visit with a sleep physician who may recommend a sleep study to assess the effectiveness of the MAS. In some sleep studies the appliance is worn for half the night and not worn for the other half of the sleep study.
Subsequent reviews: I like to review patients at six months and then yearly there after to monitor any changes, even if the patient has their own dentist.
